A very recent study has been released that feminists are treating as the smoking gun; proof of not only systemic misogyny, but that the medical system doesn’t care about women’s needs. This study is the proof they need to show that everything else they say is correct, because if one thing is proven true, then everything else by proxy of them saying it must also be true.
“Association of Surgeon-Patient Sex Concordance With Postoperative Outcomes (2022)” looks at the outcomes of patients and their surgeons based on gender, and whether or not there was any post-surgery complication. What is quoted from this study is that when women are treated by a male surgeon, there is 15% more complication than if a male or female surgeon treated a male patient.
Some on social media confound this as “Men’s health is taken more seriously and female health is not”. We all know that is bullshit.
In this article, I am going to look at the study in greater detail and demonstrate some of its flaws, and more to the point that this isn’t the revelation that feminists have been hoping for and in fact does more for the Men’s Movement.
Flaw #1 – Location
Location is everything, and when it comes to studies, the location is important to know. Certainly, taking a small sample of the Earth can still inform us of those around the world, but it shouldn’t be seen as a fact of life. Rather, more studies should be done to determine if the results remain true.
Of course, that’s common sense. You’ll look at this and say, “duh!” Yet, the feminists are taking this study (done in Ontario, CA from 2007 to 2019) as a representation of the entire world. At best, the result of this study shows what healthcare looks like in Ontario. Now, yes, it could be a representation of the world, but it may also not be. Compared to the United States of America, Canada is seen as socialist healthcare. This study focused on the Ontario Health Insurance Plan, which is a single government payer.
Flaw #2 – Procedure Process
When it comes to surgery, there are a lot of steps before and after the procedure. Yet, this study focuses on one part of that process. It could arguably be the most important, with a close second being recovery, and third being pre-surgery preparation. No matter how good the operation was, problems can still occur from non-surgeons that are still linked to the surgery.
Now this is a flaw that the study noted:
“Third, we are unable to account for the potential influence of residents, nurses, and other physicians apart from the primary billing surgeon of record on patients’ outcomes. This represents a valuable avenue of future work to understand how these additional members of the health care team may either strengthen or impair the patient-surgeon relationship. We noted a consistent association of sex discordance across academic and community hospitals, suggesting that resident teams are unlikely to dissipate this effect.”
They’re aware that their study is limited in this way, not that feminists or the media point that out. Even then, they are quick to twist it around and state that they don’t think the additional staff makes a difference to their findings. It would seem to suggest that the primary surgeon is the only person important to the process.
Flaw #3 – Cases
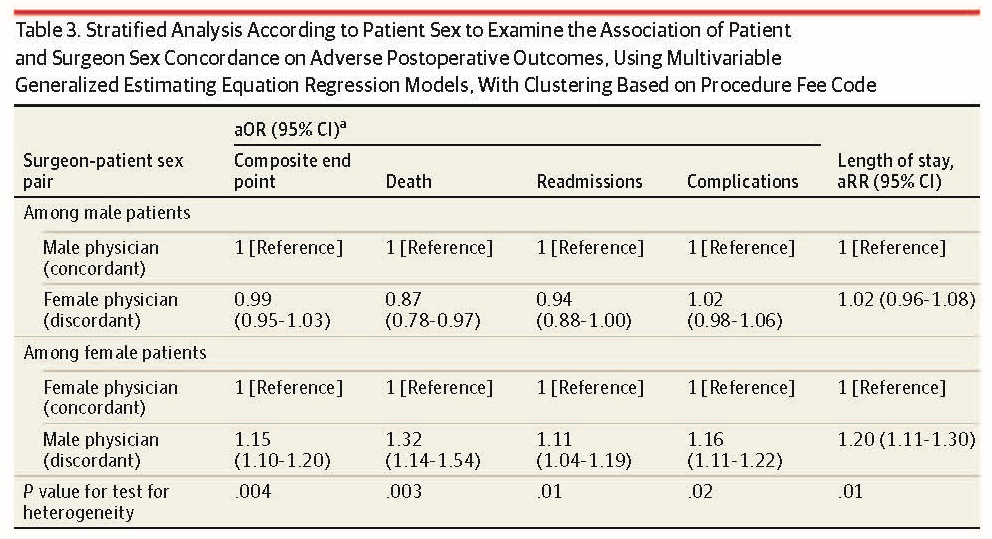
While starting with 1,870,221 procedures during the timeframe, they limited the study to first-time surgeries and removed non-surgical doctors, patients under 18, non-Ontario residents, multiple surgeries on the same day, gender-specific surgeries, and those whose full medical data was not able to be properly linked. The remaining cases totaled 1,320,108.
This was divided into 2 categories: Sex Cordant (same sex doctor and patient) and Sex Discordant (different sex doctor and patient). This divided the cases into four subcategories:
- Male Surgeon, Female Patient (667,279)
- Male Surgeon, Male Patient (509,634)
- Female Surgeon, Female Patient (92,926)
- Female Surgeon, Male Patient (50,269)
One thing to notice right away is that male surgeons saw 89% of the patients in this study, with female surgeons seeing only 11%. We are talking about thousands of cases, but this is a ratio of 8:1, or for every 8 surgeries done by men, 1 was done by a woman. Or, men performed 821% more surgeries than women.
I’m sure someone will point out that an adjusted odds ratio (AOR) was used, which is basically taking the female surgeon sample size and calculating to what it would probably would look like if there were as many surgeries as men performed. That is a normal procedure done for studies. Understand, however, that this is a prediction. Nothing wrong with predictions, but we are talking a sizeable difference of 1,033,718 surgeries. Yet, this is treated as absolute fact by the feminists.
Let me demonstrate this another way. Below are three pictures. The first is a 10×10 picture (100 pixels). I then increased that to 31×31 (961 pixels). This is about 10 times more. Using the same font, I made a third picture at 31×31 and we see the difference between the two. In order for the first image to be upscaled to the second, the software had to create 861 new pixels to maintain the shape, but as we see, it is quite blurry. Now we can understand it is an M, but we see that it is just a prediction by the software and far from accurate of what it should look like. There are of course software out there that can make a better prediction of what it should look like, but the more extreme the difference is between initial size and the resize, the less accurate it will be overall.
As I said, AOR is a standard done in studies and often times we have to use predictive algorithms to discern what to expect along a logical path, but this shouldn’t be taken as absolute fact. I argue though that the greater distance between the numbers, the more skeptical we should be, and a 1 million number difference makes me extremely skeptical. In my opinion, this gap is too wide for this to be discerned as fact and more of a case of further study.
Flaw #4 – Specializations
Like the wage gap that took all earnings and compared men versus women, this study looks at all specialties as one. As we know, when we look at specific industries for the wage gap study, there are many that are female dominated with women earning more than male counterparts, and when we adjust for variables, such as work history and education, the wage gap disappears.
Surgical specializations included in this study were: Cardiothoracic, General, Neurosurgery, Orthopedic, Otolaryngology, Plastic, Thoracic, Urology, and Vascular. All of these fields are male dominated, with female dominated fields being Pediatrics and Obstetrics/Gynecology (two fields not included). Of the patient cases shown in this study, female surgeons are more represented in General surgery (21% female) and Orthopedic surgery (4% female). I’m sure a feminist will state that these are boys’ clubs and women aren’t allowed, but if that was true, then how are there so many patients with female surgeons?
The significance of this is risk.
Flaw #5 – No Measure of Risk
More women are in general surgery than all other paths in this study. Let’s dive a bit deeper. The mean age for male surgeon is 41–56, versus women who are 37-49. Men spend 7–22 years practicing and women 4–17. This tells us that men are more likely to make surgery a lifelong career versus women, or at least stay in the field longer. Adding to that, male surgeons can take on 15 times more cases than female surgeons do.
While the study believes that men don’t necessarily take on more riskier procedures than women, I would disagree. Men stay in longer, take on more cases, dominate in non-gendered specialty fields, and also do surgery on older patients (52-73 vs 39-70).
Let’s flip this around: female surgeons stay in surgery for a short time, tend to stay in fields that are female specific or less specialized, and work with younger patients.
The one thing this study doesn’t assess is what was the risk prior to surgery. The closest that they do show is comorbidity, which can tell us what kind of problems a patient had including the reason they go into surgery. Male surgeons tend to have patients with higher number of comorbidity than female surgeons.
I won’t say that any surgery is easy. Going under the knife can lead to all sorts of complications. Certainly, there is a difference between walking on a curb and not falling and walking on a tightrope and not falling. You understand that tightrope walking carries greater risk. Not understanding the level of risk prior to a procedure doesn’t give us the full picture. Did male surgeons take on riskier procedures than females? The signs seem to point to yes.
Flaw #6 – Male Patient Standard
This isn’t exactly a flaw of the study but rather a flaw in the interpretation of the study. The big finding is that women are 15% more likely to have complications from surgeries if their surgeon is a man. I saw a feminist who thought that this meant that the medical system didn’t take female medical issues seriously and that males were the standard. Obviously ignoring female specific medical departments and no medical department dedicated to men. They ask, “If the study is wrong, then why don’t men have complications from male surgeons?”
The answer is: they do.
This study sets male surgeons with male patients’ complications at a value of 1, then looks at female patients’ complications and reports the increase, in this case 1.15 overall. In the case of death, it was 1.32 or 32% greater. They did the same thing with male patients, treating male surgeons as one and looked at female surgeons. Overall it was .99, and for deaths .87. This means that males did 1% better with female surgeons and were 13% more likely not to die compared to male surgeons.
This of course is a very small percentage and that’s why it’s not mentioned to the public, but the study does fail to report that males also have complications and not just female patients.
Conclusion
Understand that I don’t think the medical system is perfect. In fact, I believe that it is in need of serious reform and perhaps even be rebuilt from the ground up. There is too much corruption, outdated thinking, insurance made to deny people help, specialists who seem incompetent, and the list goes on and on.
I firmly believe the worst aspect to the system is not even the medical staffing, but the non-medical staffing. It’s basically the same as HR, and is likewise overwhelmingly staffed by women. I think a lot of people avoid the doctor because they get sick of dealing with the staff that doesn’t seem to know how to do their jobs, expect you make sacrifices for them, mess up the billing, and if you are even 5 minutes late they chastise you even if the doctor is running an hour behind. And they always want you to come in 30 minutes early. How about you set my appointment for when you want me to come in. Of all the problems of the medical system, that is definitely in the top five.
In regards to this study, in using the adjusted odds ratio I will say they manipulated their findings or rather ignored key components to make the adjusted prediction to their liking. They focused on one city, had a million-patient gap, didn’t access risks, didn’t take age and experience into consideration, didn’t consider amount of workload, and didn’t look at other responsible parties.
Is there an issue of female patients having lower standard of care with male doctors? Maybe, but this study did a poor job in trying to represent it. Other studies they used do seem to show this as a problem. For instance, there is a problem of self-reporting to male surgeons. Studies show that female patients report less problems to a male surgeon than a female one. Female surgeons are better at picking up more issues from female patients than even male doctors are from male patients. If a surgeon doesn’t know everything going in, that is likely to lead to complications. Had the surgeon known about it, they might have done something about it.
This study was narrowly focused on correlation and passing it off as causation. They admit their limitations on this, but they are quick to throw out anything that could really explain the problems such as greater risk involved or the influence of other parties.
For me, this study demonstrates that male surgeons tend to work harder and longer than their female counterparts as a whole. There might be special exceptions, but this showed that women tend to take a more risk-avoidant path than men, focusing in general areas, younger patients, and less casework. This further tells me that when we think of the wage/earnings gap, this study shows that men take on more work in harder fields and thus disproves that men are paid more for having a penis.